MIPS 2020 Final Rule & Future Planning
MIPS 2020 Final Rule & Future Planning
The Centers for Medicare and Medicaid Services (CMS) released its Final Rule for the 2020 Merit-based Incentive Payment System (MIPS) program. The Final Rule continues to gradually increase the reporting requirements and financial impact of the MIPS program. Below we share the most relevant changes that will impact your 2020 MIPS performance and help you plan for the future.
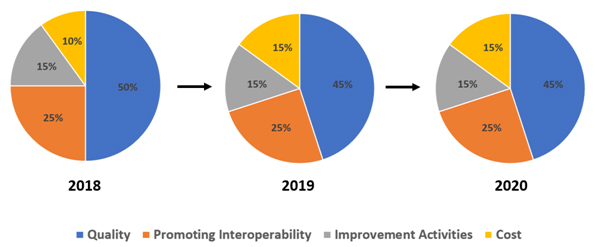
MIPS Performance Categories
In 2020, the MIPS category weights remain the same as in 2019.

2020 MIPS Categories
|
Quality |
Promoting Interoperability |
Improvement Activities |
Cost |
|---|---|---|---|
|
45% |
25% |
15% |
15% |
MIPS Reimbursement Overview
There will be larger incentives for 2020 performance year due to the higher thresholds and other changes to the program. The clinicians who are taking the program seriously will see more revenue going forward. On the other hand, those who are not taking the program seriously or have just met the bare minimum threshold in the past will have a challenging time and may see higher penalties in the future.
The lookback period is two years. Prepare in 2020 for payment adjustment in 2022.
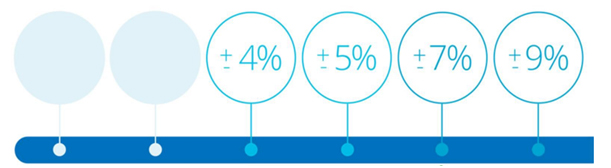
Performance Threshold & Financial Impact
In 2020, CMS increases the minimum performance and the exceptional bonus thresholds. Additionally, there will be greater financial implications for MIPS eligible clinicians who choose not to report.
| 2019 | 2020 |
| 30-point performance threshold | 45-point performance threshold |
| 75-point exceptional performance threshold | 85-point exceptional performance threshold |
| Maximum payment penalty set at -7% | Maximum payment penalty set at -9% |
| Maximum incentive prediction at +4.69% | Maximum incentive prediction at +6.25% |
Note:To ensure budget neutrality, positive payment adjustment is likely to be increased or decreased by an amount called a “scaling factor.” The amount of the scaling factor depends on the distribution of final scores across all MIPS eligible clinicians.
MIPS Timeline
Below are pertinent milestones for the MIPS program.
| Milestone | Date |
| 2018 Performance Adjustment | Jan 1 – Dec 31, 2020 |
| 2019 Data Submission | March 31, 2020 |
| 2019 Performance Feedback | July 1, 2020 |
| 2019 Target Review | August 31, 2020 |
| 2020 Data Reporting | Jan 1 – Dec 31, 2020 |
| 2020 Performance Adjustment | Jan 1 – Dec 31, 2022 |
MIPS Eligible Clinicians
In 2020, the MIPS eligible clinician categories remain the same as in 2019.
| 2020 MIPS Eligible Clinicians | |
| Physicians | Audiologists |
| Physician Assistants | Physical Therapists |
| Nurse Practitioners | Occupational Therapists |
| Clinical Nurse Specialists | Speech-Language Pathologists |
| Certified Registered Nurse Anesthetists | Clinical Psychologists |
| Audiologists | Registered Dieticians or Nutrition Professionals |
MIPS Eligibility Criteria
To be able eligible to participate the clinician must meet the following three requirements:
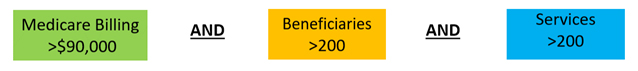
- If you are a MIPS eligible clinician and meet or exceed at least one, but not all, of the low-volume threshold criteria, you may opt-in to MIPS
- If you opt-in, you’ll be subject to the MIPS performance requirements, MIPS payment adjustment,etc.
Note:You can voluntarily report if you are a clinician or group that is not MIPS eligible.If you report voluntarily, you will receive a MIPS final score but no payment adjustment.
MIPS Performance Period
The performance periods for respective MIPS categories remain unchanged.
| Performance Category | 2019 | 2020 |
| Quality | 12 months | 12 months |
| Cost | 12 months | 12 months |
| Promoting Interoperability | 90 days | 90 days |
| Improvement Activities | 90 days | 90 days |
Changes in Quality
In 2020, the following changes are expected in the Quality category:
- CMS eliminated 42 quality measures and added 4 new measures
- The data completeness requirement increased from 60% to 70% in 2020. In other words, Quality measures will need to be reported on at least 70% of eligible cases, for both Medicare and non-Medicare patients, for the entire year. Measures that are submitted, but do not meet the data completeness threshold (even if they have a measure benchmark and/or meet the 20-case minimum), would receive 0 points (instead of 1 point in 2019).
- Clinicians in small practices (15 or less in the TIN) would continue to receive 3 points for measures that don’t meet the data completeness requirements.
- Several Quality measures have topped out or have been removed.
- New specialty sets have been added including for Speech Language Pathology, Audiology, Clinical Social Work, Chiropractic Medicine, Pulmonology, Nutrition/Dietician, and Endocrinology.
- Flat percentage benchmarks are being established for limited cases where CMS determines that the measure’s benchmark could potentially incentivize inappropriate treatment for some patients.
Changes in Promoting Interoperability (PI)
The PI category will not see any significant changes in 2020, except below:
- A group will be considered hospital-based and eligible for reweighting if more than 75% of the clinicians in the group meet the definition of a hospital-based individual MIPS eligible clinician (it is currently 100%).
- CMS will remove the Verify Opioid Treatment Agreement measure and keep the Query of PDMP measure as optional.
- Clinicians will be allowed to satisfy the optional Query of Prescription Drug Monitoring Program (PDMP) measure with a yes/no response instead of a numerator/denominator (also applies in 2019).
- The points for Support Electronic Referral Loopsby Sending Health Information measure will be redistributed to Provide Patients Access to Their Health Information measure if an exclusion is claimed (also applies in 2019).
Changes in Improvement Categories (IA)
As with Quality measures, there is a net reduction in the number of IA measures. Here are the key changes:
- 15 IA activities were removed, 2 new added and 7 modified.
- CMS increased the participation threshold for group reporting from a single clinician to 50% of the clinicians in the practice.
- The definition of rural area was modified to mean a ZIP code designated as rural by the Federal Office of Rural Health Policy (FORHP) using the most recent FORHP Eligible ZIP Code file available.
Changes in Cost
Out of the four MIPS categories, Cost category will see the most changes. Key changes are below:
- CMS is revising the current measures – Medicare Spending Per Beneficiary Clinician measure and Total Per Capita Cost measure. There will be no changes to current case minimum requirements.
- The driver for above change is to address the concern from clinicians of certain specialties that patients were attributed to them over whom they have minimal control, both in terms of their behavior and clinical outcome. This negatively impacted the Cost score of the specialist clinician. The 2020 changes in patient attribution methodologies is expected to positively impact the Cost score for the impacted clinicians.
- 10 new episode-based measures have been introduced, increasing the total number of such measures to 18.
MIPS Value Pathways (MVP)
In order to reduce the MIPS reporting burden on clinicians, CMS is adopting a new framework beginning in 2021 performance year called the MIPS Value Pathways. (MVPs) Under MVPs, clinicians would report on a smaller set of measures that are specialty-specific, outcome-based, and more closely aligned to Alternative Payment Models (APMs).The goal of MVPs is to reduce the reporting burden by moving towards an aligned set of measures more relevant to a clinician’s scope of practice across all MIPS categories for different specialties or conditions.
Here is a CMS video explaining the MIPS Value Pathways framework. (Source https://qpp.cms.gov/mips/mips-value-pathways)
Planning for 2020
MIPS eligible clinicians and groups should continue to stay on top of their 2019 MIPS data reporting, and at the same time become familiar with the changes for MIPS in 2020.The 2020 final rule establishes higher performance thresholds and payment adjustments, so more planning and reporting will be necessary to avoid any penalties.
TriumpHealth consultants help you with acquiring pertinent MIPS knowledge, planning, and monitoring performance. To see how we can help you maximize incentives please click here or call us at (888) 747-3836 x1.
By Tej Gill – VP Healthcare Solutions, TriumpHealth
References:
Recent Posts
- Proven Strategies to Maximize Patient Retention
- Importance of Provider Credentialing in Establishing a New Medical Practice
- Why Healthcare Providers are Choosing to Outsource Medical Billing and Revenue Cycle Management
- Credentialing Relief
- Addressing Security Risk in Healthcare Organizations
- Increasing Revenue via Better Patient Engagement