MIPS FAQs
by browsing through our FAQ section
MIPS FAQ’s
What is MIPS?
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) repealed the Medicare Part B Sustainable Growth Rate (SGR) reimbursement formula and replaced it with a new value-based reimbursement system called the Quality Payment Program (QPP). The QPP consists of two tracks:
- The Merit-based Incentive Payment System (MIPS)
- Advanced Alternative Payment Models (Advanced APMs)
The focus of this FAQ is on MIPS as a majority of eligible providers will be reporting through the MIPS track.
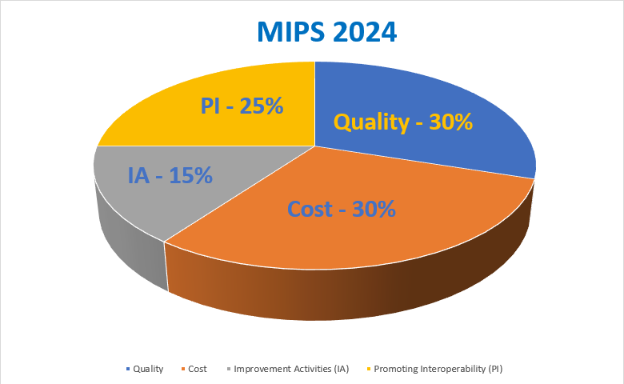
MIPS will measure eligible providers in 4 performance categories to derive a final MIPS composite score of “0 to 100”. The 4 categories with their individual assigned scores in 2024 are:
- Quality = 30%
- Promoting Interoperability (PI) = 25%
- Improvement Activities (IA) = 15%
- Cost = 30%
How does MIPS work?
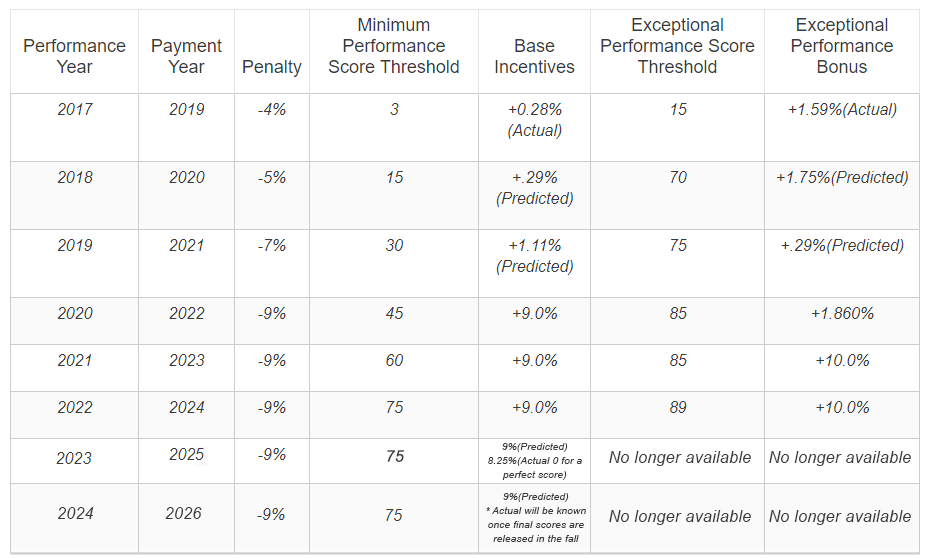
MIPS is a composite score based payment system such that higher score results in the potential for higher incentive and vice versa. Thresholds have been set for clinicians to meet and avoid a negative adjustment, while exceeding the threshold may result in a positive adjustment.
What is the financial impact of MIPS?
MIPS will financially impact Medicare Part B providers by a performance adjustment that will be seen on every reimbursement. The negative or positive adjustment received is solely based on the eligible clinician’s performance across the 4 reporting categories.
How will MIPS affect your practice or healthcare organization visibility?
The reputational impact of MIPS makes it even more important for you to understand where you stand today against existing benchmarks as well as what changes you can make to have the most impact on your performance, quality of care, and MIPS score.
Medicare Physician Compare Website currently shows whether the physician reported on the quality measures and used electronic health records. This website was completed September 2015 as part of the Physician Compare Initiative. The physician’s scores are available on this website, allowing patients to compare physician performance and help them make informed decisions about their care. Basically, your MIPS score will influence your visibility and reputation, which can impact patient retention and revenues.
Maximize Your Revenue. Schedule a Consultation Today!
We will help you achieve financial and regulatory compliance goals resulting in improved patient outcomes and increased revenue.



